The number of people who have lost their lives due to complications from COVID is hard to even fathom. In trying to comprehend a number over 330,000, I established that you could fill a professional football stadium five times. This number continues to grow despite the efforts of reducing risks.
I want to bring awareness to the devastating effects of isolation, as it contributes to non-related COVID deaths. The absence of family and friends is the harsh reality of the pandemic for residents in nursing homes, assisted living and in the community. It is of specific detriment to people with dementia. Most residents have been confined since March. “Long-term care employees describe increased confusion, anger, and anxiety among residents. Family members said their relatives were deteriorating in short-staffed facilities that have pared back therapies, engagement activities, and visits into the community.”
My colleagues from adult day programs, senior centers, and residential communities, have openly expressed the tragic experiences of their clients, participants, and residents. Many people with dementia have progressed to advanced stages, require more physical care, and display increasing behavioral and psychological symptoms. Many have died. Social isolation and loneliness are to blame.
Human’s most fundamental need for physical, emotional, intimate, and intellectual human contact is devoid. We are entering even darker days ahead with the suggestion that these next few months will be the worst we have seen in terms of number of deaths related to COVID.
Engagement with peers, family, and friends creates the socialization that directly slows down a dementia disease process. In my experience, socialization and purposeful engagement are the most important treatments for dementia. As a Dementia Specialist, I educate care partners on how to provide the daily opportunity for purposeful and meaningful engagement. This is what improves the quality of life for people with dementia. The lack of structure and routine decreases one’s sense of safety, security, and comfort.
As nursing centers and assisted livings receive the vaccine, we must begin to prioritize efforts to decrease the loneliness and isolation. Nursing homes need to focus on each resident and what can be done in terms of increasing functional independence. Physical and Occupational Therapists must be part of the care plan to regain as much independence as possible. Engagement opportunities must resume including re-instituting outside services, such as, musical entertainment, pet therapy, intergenerational activity, and many others.
Engagement for a person with dementia must be successful, failure-free, and purposeful. This includes physical exercise, creative opportunities, intellectual offerings, music and rhythm, sensory fulfillment, household specific jobs, and revisited positive past experiences.
The decline includes weight loss, and this too is a result of isolation. Specifically, people with dementia have better nutritional intake when participating in socialized dining. Eating is a social activity. There is group mirroring that exists when eating together. They eat as they see others eat. It is the success of mirroring that encourages the functional independence of eating.
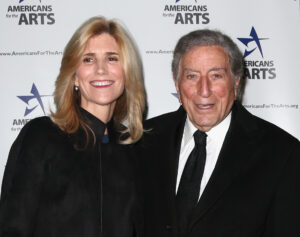
The pandemic has robbed people of potential moments of much needed human connections and engagement. If you could benefit from a free consultation to discuss the need for assistance in your organization or at home to create a structured purposeful, successful, and meaningful day of engagement for the person with dementia, please contact Tammy .