During these days of the COVID-19 pandemic, increasing violence, and political uncertainty, I wanted to talk about something else. I want to increase awareness about the reality that symptoms of dementia could very well be the consequence of something that is treatable and reversible. Dementia is NOT a diagnosis. It is a group of symptoms including memory loss; confusion and disorientation; lack of insight and poor judgement; challenges with sequencing and performing tasks; challenges with language and word finding; and mood and personality changes.
When someone experiences any of these symptoms, a common reaction is to begin to withdraw and deny what is being experienced. The underlying cause of the experienced symptoms may treatable and reversible. It is so very important to undergo a medical neuropsychological diagnostic workup. The fact is that something is causing the dementia symptoms. Yes, the diagnosis may be Alzheimer’s Disease or another Major Neurocognitive Disorder. However, the diagnosis may be a nutritional deficit, infection, or untreated Clinical Depression. The bottom line is that if anyone assumes it is a dementia disease process, there is a huge disservice for the individual.
Despite recent legislation in Massachusetts making it mandatory for physicians and nurses to receive education regarding dementia, the practice of diagnosing “Dementia” and prescribing Aricept still occurs prior to any investigation of the cause of the experienced symptoms. If I knew there may be a treatable condition causing my symptoms, I would want to know. I was training a group of research professionals and one explained how they had a 59-year-old man who displayed dementia symptoms wanted to join a drug trial. Prior to acceptance into the trial, he went through a diagnostic workup. The battery of tests performed rule out what may in fact be treatable causes of dementia symptoms. His test results showed that he was significantly Vitamin B-12 deficient. What a welcomed surprise for him to learn he did not have Alzheimer’s or other dementia. He was treated for his deficiency and no longer experienced dementia symptoms.
Prior to my training and consulting business, I owned and operated Pleasantries, now Better Day Adult Day Program in Marlborough, MA. A daughter enrolled her Dad at Pleasantries and reported him to have Alzheimer’s Disease. I conducted a thorough assessment to get to know who he was. He owned and operated a barber shop. He was the primary caregiver for his wife who was diagnosed with Alzheimer’s Disease. His wife died two months prior to his enrollment at Pleasantries. He now lived alone. He had so much loss including, the social aspect of his profession, the long journey of grief with his wife; along with, the loss of his purpose as a caregiver.
He was clearly suffering from Depression and I asked his daughter to have him receive a diagnostic workup. She assumed he had Alzheimer’s Disease like her mother as he displayed the many symptoms of dementia. The results of his workup showed Major Depressive Disorder for which he received an anti-depressant medication. He attended the day program three times per week. His dementia symptoms reversed. The treatment of the underlying cause was both pharmacological (anti-depressant medication) and non-pharmacological (socialization and purposeful engagement.)
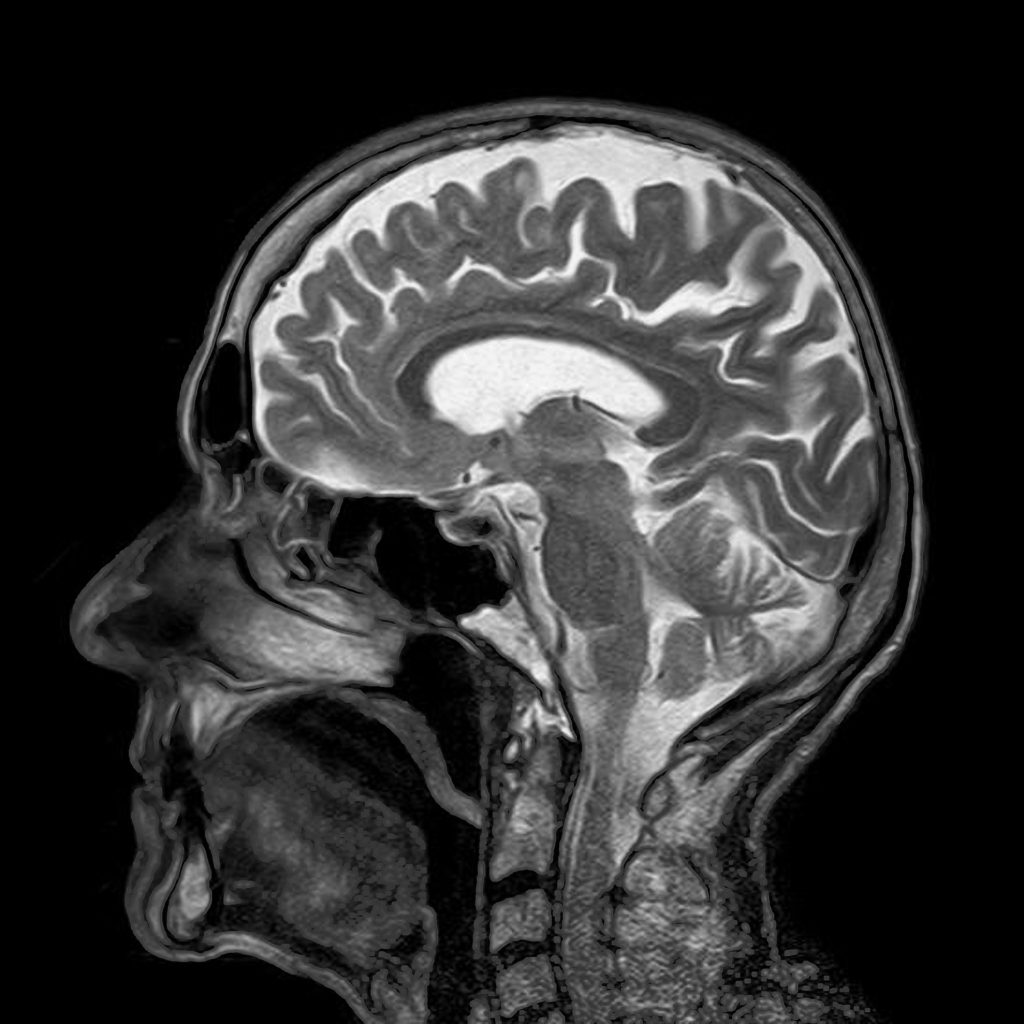
In my career, I have seen many cases where the symptoms of dementia were considered normal as a part of aging. Unfortunately, there is also the factor of having a misdiagnosis. What is wrong with getting a second opinion? I encourage it. During my time as a Memory Care Director at a nursing home, I had a 76-year-old woman resident who received a diagnosis of Alzheimer’s Disease. Her family pushed for a second opinion. Upon receiving this second opinion, Normal Pressure Hydrocephalus was discovered. If found early enough, the procedure of placing a shunt allows for the release of the cerebral spinal fluid trapped on the brain. Although there was some permanent brain damage, she was able to rehabilitate to the point where she could function high enough to return went home and live with her family. I think of this often and imagine what would have been if she did not receive that second opinion.
We should acknowledge those refusing to receive a diagnostic workup may be in denial as well as have intense fear of the possible diagnosis of Alzheimer’s Disease or other dementia disease. I encourage you to validate and empathize those feelings; however, focus on the potential treatable and reversible underlying condition. Do not give up encouraging your patient, client, resident, guest, or loved one to receive a diagnostic workup.
You may be asking where do I go? There are many resources for medical neuropsychological diagnostic centers. One would be to contact the Alzheimer’s Association’s helpline 1-800-272-3900 and ask for the list of diagnostic centers. You may want to investigate the Boston Center for Memory, Center for Memory Health, and the Memory Disorders Division at MGH to name a few.